You Must Act Prematurely - A Mindful Approach to Dementia & Psychedelics
A few days ago a friend recommended my husband and I register for a presentation, available to view here, on New and Emerging Right to Die Options: 12 Ways to Avoid Late-Stage Dementia, given by end-of-life legal expert Professor Thaddeus Pope, JD and PhD, hosted by the Hemlock Society. of San Diego. Several hundred people joined the Zoom meeting. Dr. Pope succinctly went through current legal options someone with dementia could make to die. It had taken me several years to learn about the options he had presented in less than 30 minutes. Thank you, Dr. Pope.
Henry had already discussed the two most likely options with his primary physician: VSED and DIGNITAS in Switzerland. Currently, he is pursuing DIGNITAS, having discarded the potential difficulty and possible prolongation of the VSED process. So when Dr. Pope said, “You have to give up good days to avoid bad days,” I felt a jolt of deep knowing that this was key to coming to a better decision around WHEN.
He also said, “You must act prematurely.” Another jolt. A deep truth. A truth hard to admit when Henry says he still feels life in front of him. But as Dr. Pope also mentioned, “You have to act while you still have capacity.”
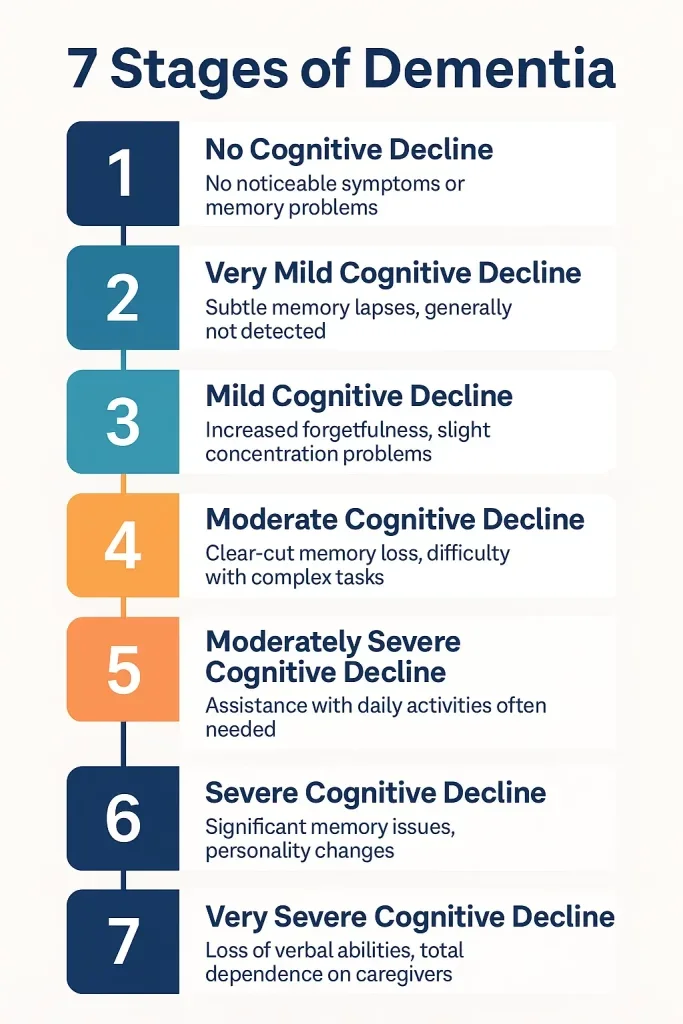
The biggest jolt came when Dr. Pope referred to the 7 stages of Alzheimer’s (not all descriptions of the 7 stages are exactly alike). When the question came up about how capacity is determined, it was the first time I learned a very specific answer. Dr. Pope said stages 1, 2, and 3 are capacity; by stage 4 it is iffy, while at stages 5, 6, and 7 there is no capacity.
So after Henry went to sleep I went onto the internet and the first image that popped up I include down below. Henry is a 4 and but increasingly a 5, according to this scale. Remarkably, in social conversation he appears to be a 1 (confusing to friends and family or disbelief that he is at a moderate stage of cognitive impairment). He is aware of decisions and the ability to express and make choices. When it comes to Alzheimer’s, nothing is black and white or follows a strict timeline or scale.
Time is running out. The honeymoon phase is over and the slippery slope is upon us.
Our two daughters, both of whom are supportive of their father’s choice to die with dignity, are calling for an emergency meeting. Although Henry has expressed that he will make his choice in 2026, he also seems less inclined to go into any further details. However, we now have a case worker from DIGNITAS. Medical records have been sent. An updated visit to the neurologist (a requirement) is happening tomorrow. We had been under the impression that since Henry’s advanced directive for MAID as a patient with Alzheimer’s had been accepted by DIGNITAS, that he was not required to have enough capacity or discernment (as referred to in the personal account of a spouse choosing DIGNITAS by journalist Amy Bloom in her best-selling book In Love) to make an informed choice.
Capacity to express the choice at the moment of receiving the lethal medicine is a must. This changes EVERYTHING. Dr. Pope’s words are now our guiding barometer. We are making what was up until now an idea into a more tangible, perceivable reality. At this time DIGNITAS is actually booking 4–5 months out. So, yes, you need to plan ahead.
This has become even more urgent in the last few days after an emergency visit to the hospital when Henry was in excruciating pain. Was it a reaction to the last medication he was trying? Henry had stopped microdosing to give one last try to a pharmaceutical. This time it was a patch, the brand name rivastigmine. The patch was changed every 24 hours. Henry’s physician thought he might tolerate it better than the other medications that he had tried, all in pill form.
It had been close to a month when he got so dizzy that he asked to have the patch be removed. He had already been getting closer to going back to microdosing as there had not been substantial benefit from the patch. Yes, at times he seemed to be more “present,” but there had been no other observable benefits. In fact, there had been a few alarming incidents including a devastating night of disorientation. His confusion and times of disorientation had been increasing.
Once again, I see microdosing having as many (if not more) benefits than a pharmaceutical; and notably, without the negative side effects. Once we get through this medical emergency, Henry hopes to return to daily microdosing. Yet we have been catapulted into the next phase of Alzheimer’s…..and the journey of the caregiver.
In the past few days I have felt broken, unable to help ease Henry’s confusion about his physical discomfort. I remember the doctor explaining when there is a physical problem when someone has Alzheimer’s, it affects the mental area as well. And at this point, all care lands squarely on me. I am glad we plan to be in Mexico in a month’s time where I will have more support. The support is both for Henry as well as for me. I am grateful that we have this choice. I know not everyone feels they have a doable option and my heart goes out to them.
What confronts my heart more than the day-to-day care is the possibility that Henry cannot make his choice in time to be eligible for the graceful exit he wants. In fact, it terrifies me. I trust, I hope, and I pray that the window of time left for Henry to have the capacity, the discernment, and the cognition to make this choice is open for him.
It is a slippery slope and the window is closing. He will have to act prematurely. This is the next part of the journey.
- Lauren Alderfer, PhD.